An 85-year-old man with severe symptomatic aortic stenosis, deemed unsuitable for surgical replacement, was referred for transcatheter aortic valve implantation (TAVI).
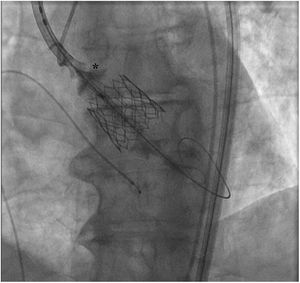
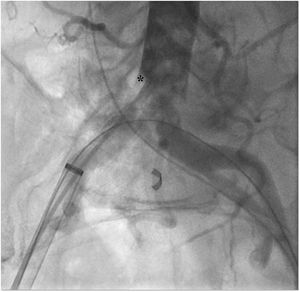
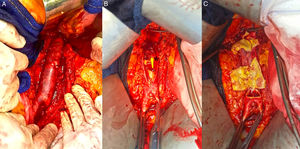
An Edwards SAPIEN 3 number 29 valve was successfully placed using a percutaneous bilateral femoral access. However, during the implantation the nose-cone balloon burst, preventing an adequate balloon deflation (figure 1). While we attempted to remove the balloon, it became stranded at the infrarrenal aorta. After several fruitless percutaneous maneuvers to retrieve the balloon using a snare device (EN Snare, MeritMedical, United States), the patient developed severe abdominal pain and an angiogram showed a dissection of the infrarrenal aorta (figure 2; *aortic intimal flap). Therefore, the patient underwent an emergency laparotomy, the infrarrenal aorta and both common iliac arteries were exposed, displaying a complete wall dissection (figure 3A). After performance of an aortic longitudinal arteriotomy, the TAVI balloon was retrieved showing a shattered aortic wall (figure 3B; TAVIs nose-cone balloon constrained in the infrarrenal aorta; figure 3C). The infrarrenal aorta was repaired using an aortic-aortic 16 mm Dacron-graft interposition from bellow the renal arteries to the aortic bifurcation.
The postoperative period was uneventful and the patient was discharged to the ward after 7-days at the intensive care unit, with a full hospital stay of 21 days. The patient made a good recovery and remains asymptomatic at the 1-year follow-up.
Although TAVI is considered a minimal invasive technique, it is not free from life-threatening complications that may require major interventions. As such, a multidisciplinary approach is essential to prevent and resolve any potential complications.