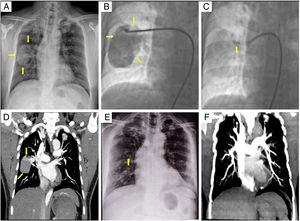
A 48-year-old man was referred to our hospital for percutaneous closure of a pulmonary arteriovenous fistula (PAVF). The patient's history included a 1-year history of hypertension, pulmonary tuberculosis in 1985, cerebral infarction in 2012, and a 10-month history of dyspnea on exertion. Chest X-ray showed a homogeneous mass in the right lower zone measuring 5.2×7.5cm (figure 1A, arrows). Arterial oxygen saturation was 88.3% at rest. Selective right pulmonary angiography revealed PAVF (figure 1B, arrows and ). PAVF is an abnormal direct connection between the pulmonary artery and pulmonary vein. Most PAVF are congenital and acquired PAVF is rare. This patient had an acquired PAVF secondary to tuberculosis infection. Treatment for PAVF includes surgical resection of the affected lobe of lung and transcatheter interventional closure.
Based on the size and anatomic features of the feeding artery, which was identified by selected pulmonary artery angiography, the PAVF was closed with a 10-mm vascular plug (figure 1C, arrow and ). Its diameter was 4mm larger than that of the feeding artery. Subsequently, the patient's arterial oxygen saturation level increased to 95%. Computed tomography pulmonary angiography (CTPA) showed vascular aneurysm with a small amount of contrast medium (figure 1D, arrows) 1 day after closure. The patient took aspirin for 1 month after the procedure. Five years later, he was doing well and had no dyspnea symptoms. Chest X-ray showed an occluder shadow in the right hilum of lung (figure 1E, arrow) and no PAVF. Pulmonary artery stenosis was identified by computed tomography pulmonary angiography (figure 1F).
FUNDINGThis work was supported by Projects of the National Natural Science Foundation of China [81360037 and 81700438].
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2020.01.006