We present the case of a 68-year-old man with multiple cardiovascular risk factors and a past history of acute non–ST-elevation myocardial infarction who was evaluated for episodes of atypical central chest discomfort with postprandial exacerbation and dyspepsia. Progressive angina was suspected and the patient was referred for 2-day stress and rest myocardial perfusion imaging with the vasodilator regadenoson.
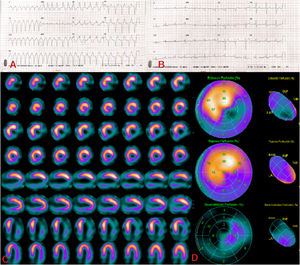
After administration of regadenoson, the patient developed regular tachycardia characterized by wide QRS complexes and a heart rate of 125 to 140 beats per minute (figure 1A). The tachycardia reverted to sinus rhythm within a few seconds (figure 1B), suggesting nonsustained ventricular tachycardia. Once clinically and hemodynamically stable, the patient underwent single-photon emission computed tomography (SPECT-CT).
The stress images showed extensive severe hypoperfusion in the lateral, inferior and apical regions. As can be seen in the short, long vertical, and long horizontal axis slices (figure 1C) and the polar maps (figure 1D), these defects were partially reversible at rest (figure 1D). Gated SPECT imaging showed moderately decreased systolic ventricular hypertrophy and an ejection fraction of 55% under stress and 61% at rest. These findings were consistent with inducible ischemia and possible nontransmural necrosis, with viability in all myocardial segments. Subsequent coronary angiography confirmed multivessel disease amenable to revascularization.
Serious adverse reactions to regadenoson are uncommon and include ventricular arrhythmias, which are potentially fatal and poorly documented in the literature. In the current case, ventricular tachycardia was due to ischemic damage, probably due to a reentry mechanism in the damaged areas of the heart.
Informed consent was obtained from the patient for publication of this article.
FUNDINGThe article did not receive any funding.
AUTHORS’ CONTRIBUTIONSAll the authors revised the text. M. Moreno-Caballero conducted the study, reviewed the literature, and drafted the manuscript and revised the final version. E. Moratalla-Aranda and A.C. Villena-García oversaw the writing of the manuscript and revised it in full.
CONFLICTS OF INTERESTThere are no conflicts of interest.