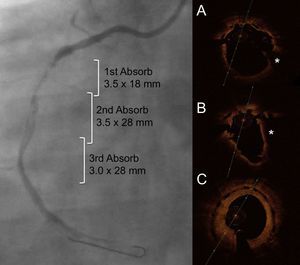
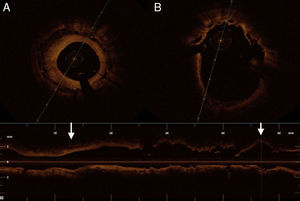
A 39-year old man with a history of inferior ST-elevation myocardial infarction underwent primary angioplasty with implantation of 3 overlapping bioresorbable scaffolds for long right coronary artery disease. After 17 months, and while on treatment with aspirin and clopidogrel, he had a new inferior ST-elevation myocardial infarct; thrombosis of the proximal scaffold was seen on coronary angiography (Figure 1). Optical coherence tomography was performed, which showed correct expansion and apposition of the second and third scaffolds, maintained in the area of overlap, with excessive neointimal proliferation (Figures 1C and 2A). In the area of thrombosis, a large quantity of red thrombus was seen (asterisk), with struts showing a thinner endothelial covering; at the level of the occlusion, malapposed and underexpanded struts were seen, with absence of endothelial covering (Figures 1A, 1B, and 2B). Heparin and abciximab were administered, and after successive thromboaspirations, the malapposed segment with significant restenosis was postdilated, a drug-eluting stent was implanted at this level, and clopidogrel was switched to prasugrel.
This case illustrates a very late thrombosis in a bioresorbable scaffold, whose possible mechanisms were malapposition and underexpansion of the proximal scaffold, which coincided with the area of occlusion of the first infarct. The cause of this malapposition and of the struts not being covered could have been the residual thrombus. Notably, there was significant restenosis in the third scaffold (Figure 2A), in contrast with the lack of endothelialization of the most proximal scaffold (Figure 2B), as well as the presence of almost all of the struts, 17 months after implantation.