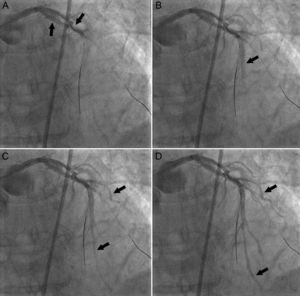
A 69-year-old woman with hypertension was admitted for an acute coronary syndrome. Emergency coronary angiography showed a long, bifurcated, calcified lesion in the left anterior descending artery (LAD). An interventional procedure was performed by predilations with an expandable and a nonexpandable balloon. Following the last inflation, angiography showed LAD occlusion due to a perforation, which resulted in an arteriovenous fistula toward the anterior interventricular vein (Figures A-D, arrows: sequential images showing passage of contrast from the LAD to the anterior interventricular vein). Guide wires placed in the LAD and diagonal branch [video 1] caused the perforation leading to cardiac arrest due to ventricular fibrillation, from which the patient recovered after 2 defibrillation shocks and cardiac massage.
Prolonged balloon inflation was performed in the area of the rupture and 50 mg of protamine was administered. After confirming that the perforation had sealed, 4 drug-eluting stents were implanted in the proximal-medial LAD. Following implantation of the last stent, the patient became clinically unstable, coincident with a diffuse ST-segment elevation in the precordial leads, secondary to extensive stent thrombosis (video 2). This was successfully resolved with reheparinization, intracoronary abciximab and balloon inflations. The patient has remained asymptomatic after more than 1 year of follow-up.
Coronary perforations tend to drain into the pericardium and only exceptionally into the cardiac chambers (Ellis type III cavity spilling). Coronary arteriovenous fistulas secondary to a coronary perforation are rare, with only 2 reported cases. Protamine use is controversial, although supported by experts, and it produced stent thrombosis in our patient. Deferred revascularization or the use of coated stents to seal the coronary perforation would have been valid alternatives to avoid protamine use and the resulting risk of stent thrombosis.