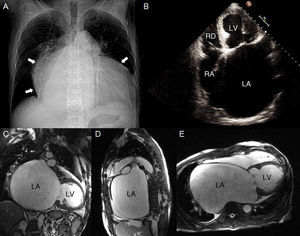
A 76-year-old man with a history of chronic mitral regurgitation presented with symptoms of progressive heart failure. The chest radiograph (Figure 1A) showed severe cardiomegaly (arrows), with a cardiothoracic index (CTI)>0.7. Echocardiography (Figure 1B) demonstrated severe biatrial dilatation, severe mitral regurgitation consistent with rheumatic valve disease, and moderate aortic and tricuspid regurgitation. Since the patient refused preoperative coronary angiography, an isotope stress test was requested. The study showed no myocardial ischemia, but a large photopenic area was seen in the right mediastinum. Cardiac magnetic resonance imaging disclosed a giant left atrium (GLA) with a calculated volume of 2100mL (Figure 1C–E) and severe mitral regurgitation with a regurgitant fraction of 46%. The patient underwent surgery, which involved triple valve repair and reduction of the size of the left atrium.
Figure 1.
Currently, GLA is an uncommon diagnosis because the frequency of rheumatic valve disease has decreased over recent years. Classically, GLA is defined by a CTI of ≥0.7 on chest radiography. Echocardiography is the imaging technique of choice in these patients because of its precision in assessing the heart chambers. Nonetheless, cases such as ours have been described in which echocardiography may not be sufficient to define accurately the atria and adjacent structures. Thus, computed tomography and magnetic resonance imaging have been considered as additional techniques for this purpose, particularly in patients with a CTI>0.7.
Corresponding author:. moral.sergio@yahoo.es